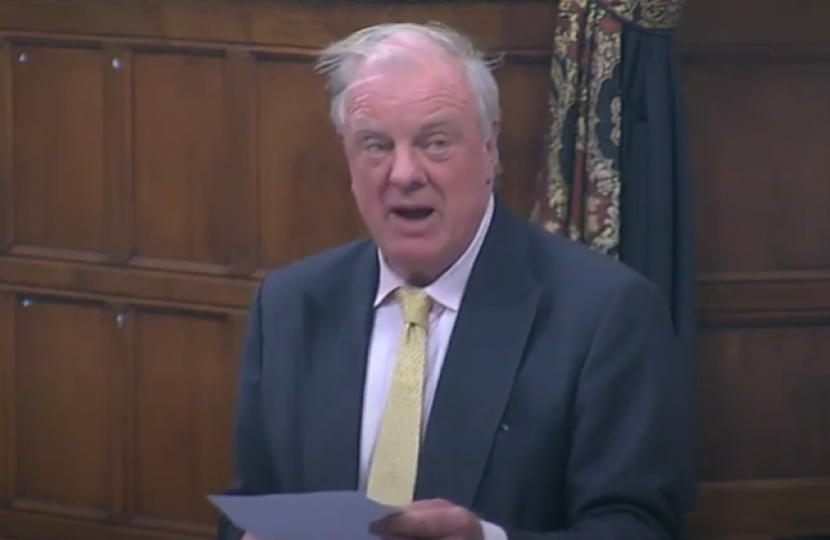
Sir Edward Leigh revealed the verbal abuse he had suffered from his skin condition in a debate on dermatology and mental health.
Speaking in a debate he had organised on skin conditions and mental health, Sir Edward said "I have rosacea, which makes one’s face red and can ultimately deform it, and I take antibiotics every day. There are many more serious conditions—I do not make a great thing of it—but only today, in relation to something else I said on a completely different subject in the House of Commons, I have already received one email accusing me of being a red gammon head and a ruddy-faced buffoon."
The video and written record of Sir Edward's speech are available below.
The written transcript of Sir Edward's speech:
I want to start my speech by making a point that I will make at the very end: mind and skin are linked, and we have to take action on both if we are to break the vicious cycle of psychological harm. I suppose, really, I should declare an interest right at the beginning of this debate. It is not a financial interest but a personal interest: I have rosacea, which makes one’s face red and can ultimately deform it, and I take antibiotics every day. There are many more serious conditions—I do not make a great thing of it—but only today, in relation to something else I said on a completely different subject in the House of Commons, I have already received one email accusing me of being a red gammon head and a ruddy-faced buffoon.
I take it very lightly, because I know I am already old and ugly, but for young people this kind of personal abuse about their appearance is deeply upsetting and drives many people into deep psychological harm, because mental health and physical health are intrinsically linked. Knowledge of this link has driven recent advances in NHS service delivery and underpins much of the thinking in the long-term plan. Although that has led to the development of trailblazing and new services for many people with long-term conditions, for some reason people living with skin conditions continue to have dire access to psychological services. Indeed, in 2020 the all-party parliamentary group on skin, which I chair, published a report on the mental health issues faced by people living with skin conditions. It demonstrated that the psychological impact can be severe, in terms of the effect on people’s work, education and healthcare use. We should all worry about this, as 60% of us live with some form of skin condition.
Since the publication of the report, the developing impact of the covid pandemic has inevitably made a bad situation worse. One of my colleagues—who might speak in the debate—said that he was told by his GP only recently that he might have to wait a year for an appointment about a skin condition. With many patients with inflammatory skin diseases now experiencing a 12-month wait for a first appointment with a dermatologist, the stress and anxiety experienced by many individuals has risen significantly. I therefore want to spend this debate outlining the need for commissioners and health leaders to rethink how the NHS provides psychological care for people living with a skin condition.
The APPG’s report on the mental health associated with skin conditions is available on the group’s web pages. The report was based in part on a survey conducted by dermatologists and psychologists of 500 skin patients, with evidence also collected from 100 clinicians and 16 dermatology-related charities. The report was led by experts from the British Association of Dermatologists. The survey part of the report found that 98% of skin disease patients felt that their condition affected their emotional and psychological wellbeing; yet astonishingly, all the patient representative and professional organisations providing evidence stated that the NHS mental health provision for skin was “poor” or “very poor”. In addition, over half the patients surveyed did not even realise that they could ask for help with managing the mental health impact of their skin disease. That clearly demonstrates just how under-resourced services are in this part of the NHS.
I would like to draw the attention of the House to some other worrying findings that our research for the report highlighted: 93% of patients surveyed said that their skin condition had a negative impact on their self-esteem; 83% said their skin condition negatively impacted on their sleep; 73% said their skin condition negatively impacted on their intimate relationships; and 5% said that they had contemplated suicide. Sadly, I have been informed by healthcare professionals working in our NHS dermatology services that patients living with skin conditions are at increased risk of self-harm, as we well know, and that a number of them, sadly, go on to take their own lives.
There is also a great economic impact, with the double whammy of skin disease and the psychological burden associated with it. Some patients surveyed said that their skin disease had been so distressing that they had felt they had to give up their job. Let me read a brief excerpt from a quote in the report:
“When I turned 19 it [the eczema] became so bad that I couldn’t participate in normal life anymore due to the pain…I had to give up my job as I am always too unwell.”
Of course, our skin is implicated in everything we do and it is often not understood that skin conditions affect not just the individual living with them but their wider family. As for the impact on intimate relationships, let me read out another quote from the report:
“My skin is often too painful to have intimate relations with or to even to hug or kiss my partner. I had to postpone my wedding as I can’t cope with the idea of a flare up on my wedding day.”
Recent research and evidence suggests that parenting a child with a chronic skin condition can trigger parental stress, and the all-party group’s survey also included responses from some children. Every one of the children surveyed indicated that their skin condition had negatively affected their mental wellbeing, with the vast majority reporting that it had impacted on their performance at school. One of the children is quoted in the report as saying:
“I was so depressed. I felt like I was rotting away inside an alien growth on my face. I didn’t wanna exist like that. I wanted to chop my own head off.”
All this emotional turmoil was experienced by a child living with cystic acne. Clearly, if we do not support such children, the distress that they experience in relation to their condition may have a long-term impact on their future wellbeing.
There are some good services out there. The report highlighted a few trailblazers, such as the specialist IAPT —improving access to psychological therapies—service in Sheffield and the well-established psycho-dermatology services in some London hospitals. Psychological interventions are also being tested, and approaches involving cognitive behavioural therapy, merged with mindfulness and self-compassion, are showing great promise.
Nevertheless, our report demonstrates that there is very much a postcode lottery, with many hospital dermatology services not having access to psychological services or clear pathways to refer people at risk to the support they need. Alarmingly, less than 5% of dermatology clinics across the UK are providing any level of specialist mental health support for children and young people. And believe it or not, but in Wales there are no dedicated psychological clinics, and there are certainly none in Lincolnshire. Only a very small minority of trusts have such clinics.
This is a ludicrous situation. Research shows that psychodermatology clinics are more cost-effective to run, compared with managing skin patients with psychological distress in more generalist healthcare settings. Therefore, I urge the Minister to consider how funding is allocated and spent in this area. Covid has made things worse for dermatology patients, with poorer access to face-to-face consultations further preventing assessment and identification of mental health issues.
It is not just our report that stresses the need to embed in dermatology services psychological screening and access to psychological intervention. That is also a feature of most of the recent treatment guidelines that have emerged from reviews of the academic literature and consultation with experts. For example, the recent guidelines of the British Association of Dermatologists on the treatment of the depigmenting skin condition vitiligo make it clear that access to psychological support should be available.
Furthermore, while some conditions might be primarily psychological in nature, they pretty much always present in dermatology services. For instance, skin-specific delusional conditions and medically unexplained itch disorders can be devastating, and without clear access to psychological services, such patients can be put at considerable risk of having their underlying condition go untreated. Again, recent British Association of Dermatology guidelines in this area of practice make it clear that services need to be developed to meet the needs of this specific group of patients. However, investment has not been forthcoming.
As I draw to the end of this speech, let me share another disappointing fact with the House. The all-party parliamentary group has looked into the mental health of skin patients and service provision on two prior occasions, in 2003 and 2013. Our most recent report shows that, despite a general recognition of the need for better care in this area—and leaving aside the more recent impact of the pandemic—most of the recommendations of the previous reports have, I am afraid, not been acted on by Government. That seems to ne to be an indictment of those responsible for the planning and commissioning of these essential services.
What should we do? We can start by building parity of esteem between dermatology services and other long-term conditions, both in access to specialist dermatologist care—which would of itself reduce the psychological impact—and in access to psychological services.
In order to achieve that, our report makes a number of recommendations. All NHS dermatology units must have regional access to psychodermatology services, with clear pathways for patients to be referred to for appropriate psychological intervention or support. There must be a stepped care pathway that starts with good quality screening and enables patients to speedily access the most economic and effective psychological services that they require and deserve. This is already in place for many other long-term health conditions, such as diabetes, but not for skin conditions. This cannot remain the case; it is simply not good enough.
To achieve that, we need to increase staffing in dermatology services and improve the dermatology and psychological training of all NHS staff who have regular contact with patients with skin conditions. That includes training for trainees, primary care clinicians and secondary care specialists.
Research funding for psychodermatology should be prioritised. It should focus on the development, evaluation and implementation of a range of psychological and educational interventions for patients with skin conditions. The inclusion of patient support organisations in service development is critical to amplify the patient voice and to ensure that patients have clear access to some of the excellent services available in the community. NHS mental health funding provided to local commissioners must urgently be used to invest in and improve mental health services.
In conclusion, I commend our report on mental health and skin disease, which demonstrates the alarming lack of psychological support available to people living with a skin condition. It provides national policy makers, commissioners and local service providers with an expert consensus on how mental health support for people with a skin condition should be structured in a range of clinical settings. This can be delivered cost-effectively.
The report also outlines the urgent clinical need for healthcare professionals to be equipped with the necessary skills and resources to provide the holistic care that patients need. This must include patient assessments and care that treats the mind and skin together; otherwise, we will not break the vicious cycle whereby problems create psychological problems that in turn exacerbate the skin condition. We ultimately hope that through the publication of this report and debate, the need for action will be made clear to policy makers and service commissioners working in Government and the NHS. I look forward to hearing from the Minister.


